Subcondroplasty Surgeon

Have you suffered with knee pain for more than three months, or pain that does not subside after arthroscopic surgery? If so, you may have developed a condition known as subchondral insufficiency. Subchondral insufficiency creates fractures in the bone marrow. Subchondroplasty surgeon, Dr. James Mazzara provides diagnosis and minimally invasive surgical treatment options for patients in Manchester, South Windsor, Enfield, Glastonbury and surrounding Hartford communities who are suffering from subchondral insufficiency pain. Contact Dr. Mazzara’s team today!
Subchondroplasty for Knee Pain Associated with Osteoarthritis
What is Subchondroplasty?
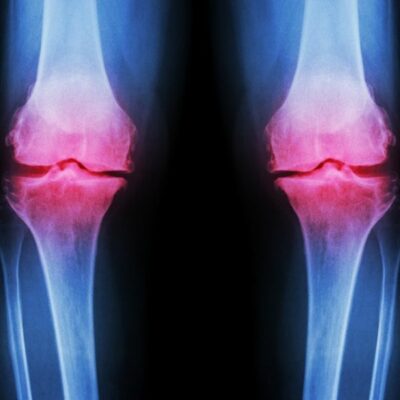
Some patients with knee injuries or osteoarthritis of the knee develop bone abnormalities called subchondral insufficiency fractures. The lesions are usually located in the interior spongy portion of the bone, the bone marrow, and can be seen on magnetic resonance imaging (MRI). Subchondroplasty is a relatively new procedure that is minimally invasive and used to fill subchondral insufficiency fractures and encourage them to heal. Dr. James Mazzara, orthopedic knee surgeon, has been successfully treating patients in Manchester, South Windsor, Enfield, Glastonbury and surrounding Hartford communities with Subchondroplasty for knee pain.
How is Subchondroplasty Done?
When the bone is under significant stress, as in the arthritic knee, the interior spongy part of the bone, called the marrow, may develop stress fractures which fail to heal further weakening the bone leading to addition fracturing. These fractures cause pain in the bone that can sometime be worse than the pain from the arthritis itself. Dr. Mazzara can perform subchondroplasty using a minimally invasive surgical technique called arthroscopic surgery. He uses a special radiological instrument, called a fluoroscope, or C-arm which provides real time x-ray images of the procedure being performed in the operating room. It is this real-time x-ray that helps Dr. Mazzara locate the exact location of the bone marrow lesion seen on you MRI and guide a needle into this area. Subchondroplasty procedure is designed to fill the bone defect with a substitute material that will harden, mimicking the body’s own natural bone. The substitute material is injected into a tiny hole drilled into the damaged area of the bone. Over time, this calcium phosphate mineral compound provides immediate strength to the bone but is eventually replaced with newer stronger bone created by the body.
Who Should Consider Subchondroplasty?
Patients who are good candidates for subchondroplasty are those who are experiencing the following:
- Discomfort when standing or walking
- Symptoms that returned after a knee arthroscopy
- Little or no relief from non-steroidal anti-inflammatories (NSAIDS)
- No benefit from physical therapy or bracing
- Symptomatic knee pain for 3 months or longer
How are subchondral insufficiency fractures diagnosed?
Bone marrow lesions are only seen through MRI and cannot be seen on a standard x-ray. Dr. Mazzara will obtain an MRI and look for damaged non-heaing areas of the bone that show stress or micro-cracks. He will also obtain a thorough patient history along with symptoms and prior injury or surgery. Every patient’s case is different and Dr. Mazzara will discuss the benefits and risks of the subchondroplasty procedure or if the patient would benefit more from a different treatment.
For more information about the subchondroplasty procedure, or to discuss your symptoms of knee pain, please contact the orthopedic offices of Dr. James Mazzara, knee surgeon in Manchester, South Windsor, Enfield, Glastonbury and surrounding Hartford communities.