Cubital Tunnel Syndrome Specialist

Are you an athlete or worker who participates in heavy lifting or heavy, repetitive tasks? If so, you may be at risk of having symptoms of paralysis in the fingers caused by nerve entrapment lesions in the elbow. This conditions is known as cubital tunnel syndrome. Cubital tunnel syndrome specialist, Dr. James Mazzara provides diagnosis and both surgical and nonsurgical treatment options for patients in Manchester, South Windsor, Enfield, Glastonbury and surrounding Hartford communities who are experiencing cubital tunnel syndrome symptoms. Contact Dr. Mazzara’s team today!
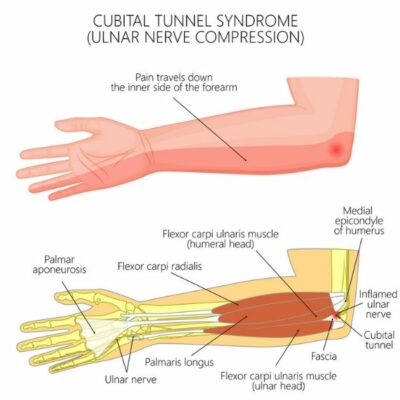
Ulnar nerve compression at the elbow – cubital tunnel syndrome
What are Elbow Nerve Conditions?
Compression syndromes of the ulnar, median, radial and musculocutaneous nerves have a number of different causes. These lesions often present with vague pain, intermittent sensory symptoms, and occasional weakness. Nerve compression syndromes can be difficult to demonstrate in the office as they often require a specific setting or activity to provoke symptoms (i.e., work, sports).
At the elbow, there is a combination of joint mobility, longitudinal stresses, and fascial restraints that make nerve compression more likely. The lack of bulky muscle and adipose tissue about the elbow makes the nerves vulnerable to direct trauma. The nerves must pass into and around the numerous muscles that originate or insert at the elbow. Anatomic anomalies such as vascular aberrations, abnormal fascial bands, boney prominences, and muscular variants are all well-documented causes of nerve compression.
Athletes and workers that perform heavy and repetitive tasks are at risk for nerve entrapment lesions because the elbow is subjected to intense repetitive muscle actions and large joint forces.
Most of the nerve injuries we see are neuropraxias which are conduction delays with an intact nerve. The prognosis for nerve recovery is usually excellent if proper treatment has been rendered before irreversible damage has occurred.
Direct trauma to a nerve may result in more severe injury in which axon degeneration occurs but the supporting connective tissue sleeve remains intact (axonotmesis). Although the prognosis is good, the time to recovery depends on the distance from the nerve lesion to the site of innervation.
Complete nerve disruption is usually associated with severe fractures, dislocations or deep lacerations and full recovery is unlikely (neurotmesis).
What is Cubital Tunnel Syndrome?
Compression of the ulnar nerve at the elbow, also known as cubital tunnel syndrome, is second only to carpal tunnel syndrome as a source of nerve entrapment in the upper extremity. The nerve can become compressed at a number of sites from 10 cm proximal to the elbow to 5 cm below the joint. The most common sites are where the ulnar nerve passes into the groove on the posterior aspect of the aspect of the medial epicondyle, in the cubital tunnel, and where it passes between the humeral and ulnar heads of the flexor carpi ulnaris muscle.
The ulnar nerve is the major nerve about the elbow most susceptible to injury due to compression, traction and repeated irritation. The superficial location of the ulnar nerve at the posteromedial aspect of the elbow contributes to frequent direct trauma. The wide range of motion of the elbow and the stresses applied during the throwing mechanism further contribute to the trauma of the ulnar nerve. In throwing athletes there are significant valgus stresses to the elbow often leading to laxity of the medial collateral ligament. This, in turn, leads to additional traction on the nerve, stretching of the support ligaments and subluxation of the nerve producing fibrosis about the nerve. Chronic symptoms also occur in individuals who put prolonged pressure on the nerve by continuously leaning on the elbow or who keep the nerve on stretch by holding the elbow flexed for long periods during work or recreation. Medial epicondylitis is associated with ulnar nerve compression in 60% of cases. Other causes of ulnar nerve compression are listed below.
What Causes Ulnar Nerve Compression?
- Compression, traction and repeated irritation
- Medial epicondylitis
- Throwing, unstable medial elbow ligaments
- Racquet sports
- Ganglia, lipoma, osteochondroma, osteophytes
- Inflammed olecranon bursa
- Rheumatoid synovial proliferation
- Occupational-related causes: accounts for 30% of cases
What are Symptoms of Cubital Tunnel Syndrome?
Early symptoms may include paresthesias in the ring and little fingers. Aching in the medial elbow with radiation proximally to the neck or distally may also occur and may extend to the ulnar side of the hand as the condition progresses. The onset may be acute and the result of an injury. More frequently the onset of symptoms is gradual and intermittent. Initially the symptoms may occur with strenuous use of the arm, but later the symptoms become more constant regardless of activity. Patients may report heaviness and clumsiness in the hand and fingers. Cramping with spasm in the ring and little fingers may occur.
Frank weakness cannot usually be demonstrated on physical examination early in the disease. Weakness of the intrinsic muscles is a late finding and can interfere with activities of daily living, such as opening jars or turning a key in a door.
How to Know I Have Cubital Tunnel Syndrome
The physical examination should start at the neck and proceed distally. The physician should palpate along the course of the nerve looking for the following:
- Supracondylar bone process
- Mass lesion
- Hypertrophy of the medial triceps
- Cubitus valgus
- Evidence of recent of past trauma
- Areas of tenderness
A Tinel sign (tapping of the nerve resulting in paresthesias down the arm) is significant only if it is strongly positive. Gentle manipulation of the ulnar nerve behind the medial epicondyle with the elbow flexed 90 degrees may demonstrate subluxation of the elbow and reproduce symptoms.
The elbow flexion test, performed by having the patient flex the elbow while fully extending the writs for 3 minutes, is positive when ulnar nerve symptoms are evoked. There is a high correlation between a positive elbow flexion test and a positive EMG. This test must be carefully interpreted and used in context with other clinical findings since 50% of normal people have similar symptoms with this maneuver.
Sensory changes in the cutaneous distribution of the ulnar nerve should be evaluated with threshold tests of vibration and light touch sensation and monofilament evaluation with Semmes-Weinstein filaments.
Nerve-ending density testing such as two-point discrimination are positive in more advanced disease.
Motor changes are seen earliest in the ulnarly innervated hand intrinsics, as may be determined by the finger-crossing test (crossing the index and middle fingers). Loss of pinch strength and Froment sign signal adductor pollicis weakness. Loss of adduction weakness ability by the little finger may be apparent on testing.
More advanced compression may produce flexor digitorum profundus asthenia in the little and ring fingers and possibly flexor carpi ulnaris weakness. Frank atrophy is a late finding and has a poor prognosis. Clawing may be evident if intrinsic wasting precedes FDP involvement.
Assessment must include evaluation for medial epicondylitis and elbow medial collateral ligament laxity. Subtle instability may be detected by comparing both elbows.
How to Diagnose Different Nerve Compressions
Cervical root compression (C8)
- Osteophytes seen on x-ray
- Herniated cervical disk: Check reflexes
- Pancoast tumor: CXR
- Thoracic outlet syndrome:Normal EMG
Carpal tunnel syndrome
Numbness in thumb, index, and middle finger
Thenar atrophy
Medial Epicondylitis
- Tenderness over medial epicondyle
- No distal weakness, paresthesias or numbness
Ulnar nerve entrapment at wrist
- Strong wrist flexors and ulnar deviators
- Sensation intact over dorsomedial hand and dorsum of little and ring fingers
Medical causes of nerve dysfunction
- Vitamin B12 deficiency
- Folic acid deficiency
- Porphyria
- Diabetes
- Uremia
- Alcoholism
- Prescription medications
- Motor neuron disease
Diagnostic Testing
Radiographic testing is of limited value. X-rays of the cervical spine are valuable when evaluating for cervical spondylosis and uncovertebral spurring. X-rays of the elbow are useful when evaluating for the presence of fracture callus, arthritic spurs, heterotopic bone, and a supracondylar process.
MRI is helpful in evaluating soft-tissue mass lesions or the status of the medial collateral ligament.
Nerve conduction velocity studies provide an objective measurement of nerve compression. A reduction in velocity of 30% or more suggests significant compression of the ulnar nerve. Nerve conduction tests may be negative in mild ulnar nerve entrapment or ulnar neuritis. Even mild compressive neuropathies may significantly compromise work-related and leisure activities.
Nerve conduction testing is particularly valuable in differentiating cervical, elbow and more distal nerve involvement.
Overall, the incidence of false negatives in nerve conduction testing is 10%. Many clinicians believe that normal nerve conduction testing should not preclude surgical treatment, nor should they be required for all patients if the remainder of the clinical assessment indicates ulnar nerve compression at the elbow.
What are Ulnar Nerve Compression Treatment Options?
The treatment of ulnar nerve compression at the elbow depends on the degree of impairment in the nerve.
Do I Need Surgery for Ulnar Nerve Compression?
Conservative measures consist of rest, anti-inflammatory medication and avoidance of the aggravating activity. Modifying activities in the workplace to limit elbow flexion and direct pressure on the ulnar nerve is the most important step in treatment. At night, an elbow splint that keeps the elbow from flexing to a right angle can be worn. A towel wrapped around the elbow at night can be used. Elbow protection pads used by skaters are available in most sporting goods stores and can be used at night with the padded part of the protector turned so that it is in the antecubital area of the elbow thus preventing elbow flexion.
During the day the sports elbow protector can be used at work to keep from bumping the elbow.
Corticosteroid injections are not recommended.
Surgical Treatment for Ulnar Nerve Compression Options
When conservative management is unsuccessful or if the severity of the ulnar nerve lesion requires operative intervention several options exist. Within our practice, one of three options are used depending on the circumstances of the case.
Medial epicondylectomy requires the excision of the medial epicondyle. By doing so the prominence against which the nerve is compressed is eliminated, and the nerve is free to seek its course of least resistance.
Ulnar nerve transposition requires that the nerve be mobilized to another location anterior to the medial epicondyle. The advantages of this procedure include the repositioning of the ulnar nerve to a bed with less scarring. In addition, the nerve is placed in a new pathway volar to the axis of elbow motion and is functionally lengthened several centimeters. This decreases tension on the nerve with elbow flexion.
The subcutaneous transposition is the procedure of choice during surgical reductions of fractures and dislocations, and replacement arthroplasties of the elbow. It is also preferred in elderly patients with arthritic elbows and in obese patients with thick subcutaneous adipose tissue.
The submuscular transposition ensures that all sites of potential nerve compression are explored and released. Its also relocates the nerve to an unscarred anatomic plane where it is not subject to traction forces. Deep to the entire flexor pronator muscle, it is well protected from compressive forces. The procedure does require more surgical dissection, and postoperative immobilization which may result in flexion contractures.
References
- Jobe, FW: Operative Techniques in Upper Extremity Sports Injuries. Mosby, 1996.
- Lubahn, JD, Cermak, M: Uncommon Nerve Compression Syndromes of the Upper Extremity. JAAOS, 6(6), 1998.
- Posner, MA: Compressive Neuropathies of the Ulnar Nerve at the Elbow and Wrist. AAOS Instructional Course lectures, 49, 2000.