Median Nerve Compression Specialist

Are you an athlete who participates in throwing sports, or are you a weightlifter? If so, you may be at risk for median nerve compression at the elbow. Median nerve compression symptoms include weakness in the thumb and forefinger, especially when gripping. Median nerve compression specialist, Dr. James Mazzara provides diagnosis and both surgical and nonsurgical treatment options for patients in Manchester, South Windsor, Enfield, Glastonbury and surrounding Hartford communities who are experiencing median nerve compression syndrome. Contact Dr. Mazzara’s team today!
Pronator Syndrome & Anterior Interosseus Nerve Syndrome
What is Median Nerve Compression at the Elbow?
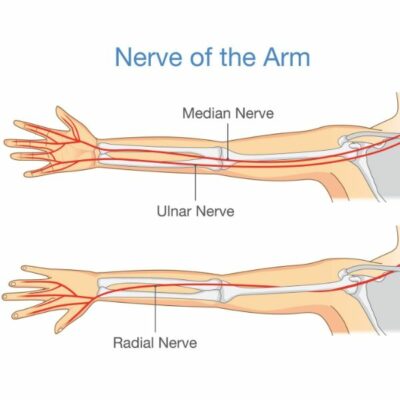
The median nerve is the least frequently entrapped nerve at the elbow. Throwing and other repetitive tasks involve repetitive forceful gripping, pronation, and sudden extension at the elbow can produce compression at the proximal margin of the pronator teres muscle. Weight lifting may result in building muscle mass and can lead to nerve compression. Trauma to the upper forearm may also result in scarring and can induce compressive neuropathies at the elbow.
The median nerve arises from the nerve roots C6 to T1. After leaving the medial and lateral cords of the brachial plexus it passes down the medial aspect of the arm to the medial humerus. The supracondylar process is a bony projection in this area that may lead to nerve compression. At this level, the ligament of Struthers may result in compression. As the median nerve enters the forearm, it courses under the lacertus fibrosis and then deep to the pronator muscle where compression may occur.
Median nerve compression at the elbow may result in two condition: pronator syndrome and anterior interosseus nerve syndrome.
What is Pronator Syndrome?
Compression of the median nerve in its course about the elbow can be produced by components of the ligament of Struthers, the lacertus fibrosis, the pronator muscle and its fibrous components, and the fibrous proximal margin of the flexor digitorum sublimus muscle.
Pronator syndrome produces symptoms of aching of the volar proximal forearm and distal arm. This aching is aggravated by forceful use of the extremity, especially involving pronation. Sensory loss in the median nerve distribution and weakness or clumsiness are often noted. These symptoms are similar to those seen in carpal tunnel syndrome. In pronator syndrome, night pain is unusual while carpal tunnel syndrome may awaken patients with complaints of aching and numbness in the hands.
What is the Physical Examination for Pronator Syndrome?
The clinical examination may reveal tenderness of the pronator teres muscle or in the region of the lacertus fibrosis in the proximal ulnar aspect of the volar forearm. A Tinel sign may be present but is often delayed in its appearance.
A supracondylar process, if present, may be palpable.
A Phalen sign (onset of numbness in the distribution of the median nerve in the hand with wrist flexion) is absent. Concomitant carpal tunnel syndrome and pronator syndrome may be present (double-crush phenomenon).
Weakness, if present, may involve the flexor pollicis longus, abductor pollicis brevis, and less often, the opponens and flexor digitorum profundus of the index and long fingers. This may present as complaints of weakness in thumb flexion and pinch strength. Atrophy in the thenar muscles may be noted in advanced cases.
Loss or decreased sensibility on the palmar side of the radial three and one-half fingers may be due to median nerve compression at the carpal tunnel. Loss of sensation in the palmar cutaneous nerve distribution (mid-palm and thenar skin) suggests compression proximal to the carpal canal.
Provocative tests on physical examination can be helpful in eliciting signs of pronator syndrome. Because compression of the median nerve by the lacertus fibrosis is a possibility, hyperflexion of the elbow past 120 degrees with resistant forearm supination may reproduce forearm symptoms if the nerve is compressed by this structure.
Resisted forearm pronation with the elbow flexed followed by elbow extension that increases symptoms suggests the pronator teres as the site of median nerve compression.
Resisted contraction of the long finger flexor digitorum sublimus may elicit symptoms if the long finger FDS is the site of compression.
How to Diagnose Pronator Syndrome
Plain x-rays are necessary to rule out a bony supracondylar process in the distal humerus or other post traumatic or degenerative pathology at the elbow as the cause for compression.
Electrodiagnostic studies (EMG/NCS) are rarely diagnostic. They may be helpful in excluding coexisting pathology and may implicate other causes of nerve compression.
What is Anterior Interosseus Nerve Syndrome?
The anterior interosseus nerve is is a division of the median nerve that branches from the median nerve approximately 5 cm below the medial epicondyle. The anterior interosseus nerve then passes behind the median nerve and then through the two heads of the flexor digitorum sublimus muscle.
Because the anterior interosseus nerve has no cutaneous sensory component, numbness is not associated with his syndrome.
Anterior interosseus nerve syndrome includes complaints of absent or decreases function of the flexor pollicis longus, pronator quadratus, and the flexor digitorum profundus of the index finger. This results in weakness or inability to flex the interphalangeal joints of the thumb and index fingers and the patient will be unable to position the thumb and index finger in the shape of a six. A weakened index finger-thumb pinch is noted.
In contrast to pronator syndrome, pain may be elicited by resisted flexion of the flexor digitorum sublimus of the long finger and may also be present at rest and on local palpation of the nerve.
How to Diagnose Anterior Interosseus Nerve Syndrome
Plain x-rays are necessary to rule out a bony supracondylar process in the distal humerus or other post traumatic or degenerative pathology at the elbow as the cause for compression.
Electrodiagnostic studies (EMG/NCS) are rarely diagnostic. They may be helpful in excluding coexisting pathology and may implicate other causes of nerve compression. EMG/NCS may be diagnostic in anterior interosseus nerve syndrome. If the EMG is not diagnostic for anterior interosseus nerve compression, one should consider more proximal causes of nerve compression such as pronator syndrome, brachial plexopathy, or a tendon rupture as occurs in patients with rheumatoid arthritis.
What are the Symptoms of Anterior Interosseus Nerve Syndrome
The anterior interosseus nerve is is a division of the median nerve that branches from the median nerve approximately 5 cm below the medial epicondyle. The anterior interosseus nerve then passes behind the median nerve and then through the two heads of the flexor digitorum sublimus muscle.
Because the anterior interosseus nerve has no cutaneous sensory component, numbness is not associated with his syndrome.
Anterior interosseus nerve syndrome includes complaints of absent or decreases function of the flexor pollicis longus, pronator quadratus, and the flexor digitorum profundus of the index finger. This results in weakness or inability to flex the interphalangeal joints of the thumb and index fingers and the patient will be unable to position the thumb and index finger in the shape of a six. A weakened index finger-thumb pinch is noted.
In contrast to pronator syndrome, pain may be elicited by resisted flexion of the flexor digitorum sublimus of the long finger and may also be present at rest and on local palpation of the nerve.
How to Treat Median Nerve Compression
The initial treatment for median nerve compression is conservative. Anterior interosseus nerve syndrome usually resolves with time, particularly is the lesion is secondary to neuritis. Observation for 8-12 weeks is favored before surgery is considered. Strengthening of the remaining muscles and modalities such as heat and stretching are useful in most cases.
If no improvement is noted, or if a space occupying lesion is present, surgical release is recommended. Decompression of the median and anterior interosseus nerve, including all suspected sites of compression, is advised.
Postoperatively the elbow is splinted for one week. After this point, flexion and extension exercises are started and slowly progressed.
The prognosis for full recovery is generally very good, provided there is no long standing muscle atrophy before surgery. Full recovery may take as long as 6 months even after surgical decompression. If there is severe nerve damage, recovery may take longer and may be incomplete.
References
- Jobe, FW: Operative Techniques in Upper Extremity Sports Injuries. Mosby, 1996.
- Lubahn, JD, Cermak, M: Uncommon Nerve Compression Syndromes of the Upper Extremity. JAAOS, 6(6), 1998.
- Posner, MA: Compressive Neuropathies of the Ulnar Nerve at the Elbow and Wrist. AAOS Instructional Course lectures, 49, 2000.