PLC Knee Injury Specialist

Are you an athlete who participates in contact sports? If so, you may be at risk of damaging your PLC. A PLC injury can occur from a blow to the inside of the knee, a hyperextension, or from a sudden stop and start. PLC injury specialist, Dr. James Mazzara provides diagnosis and both surgical and nonsurgical treatment options for patients in Manchester, South Windsor, Enfield, Glastonbury and surrounding Hartford communities who have knee PLC damage. Contact Dr. Mazzara’s team today!
Posterolateral Corner Injury of the Knee
What is a Posterolateral Corner Injury?
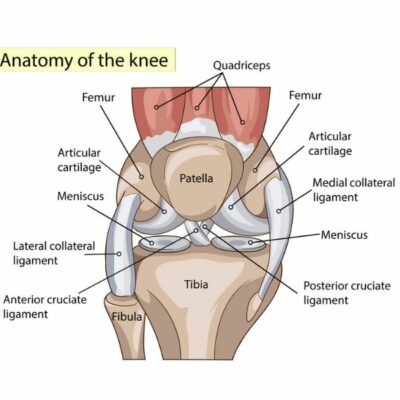
The posterolateral corner (PLC) of the knee refers to a group of structures on the outside of the knee. These structures stabilize the knee against direct lateral or external forces and include: the lateral collateral ligament (LCL), the popliteus tendon and the popliteofibular ligament. A posterolateral corner injury most often occurs with athletic trauma, car accidents and falls. Sports like football, soccer, skiing and basketball, where the knee can experience severe trauma, are often the main contributors to a posterolateral corner injury. Dr. James Mazzara, orthopedic knee specialist serving Manchester, South Windsor, Enfield, Glastonbury and surrounding Hartford communities has extensive experience in treating patients with a posterolateral corner injury.
What are the Symptoms of a PLC Injury?
PLC injuries rarely happen in isolation, but often involve other ligaments and tendons. Some common symptoms of a posterolateral corner injury are:
- Knee instability, side-to-side
- Difficulty when twisting, turning and pivoting
- Pain along the outside of the knee
- Swelling of the knee, usually will be mild
- Foot drop – common when the peroneal nerve is damaged
How is a Posterolateral Corner Injury diagnosed?
Dr. Mazzara will obtain a complete patient medical history and background including events leading up to the knee injury. Several tests can be conducted to test the instability of the knee and if an injury is present. Tests include:
- Dial Test: Dr. Mazzara determines the rotation of the knee by turning the foot outward. An increased rotation is indicative of a posterolateral corner injury.
- Posterolateral Drawer Test: With the patient lying down, Dr. Mazzara will bend the hip and the knee, checking along the outside of the knee for tibia movement (if it slides to the side while bending.)
- Reverse Pivot Shift: Another test where Dr. Mazzara bends the knee while applying slight pressure and rotation. Since some rotation is normal, he will compare the decree of shift with the healthy knee.
- Assessment for a Varus Thrust Gait: Dr. Mazzara observes the patient while walking. A stable knee maintains a straight anatomy of the femur in relation to the tibia. In a Varus Thrust, the knee moves outward while walking, giving a bow-legged look to one knee during adduction.
Dr. Mazzara will also request an MRI to see inside the joint and to determine all of the knee structures involved in the PLC injury. Careful study of the MRI will help him determine the best treatment for the patient.
How is a PLC Injury Classified?
Posterolateral corner injuries are classified using a grade system:
- Grade 1 injury: Causes minimal instability in the knee with a small, partial tear.
- Grade 2 injury: Partial tear with an endpoint to stressing.
- Grade 3 injury: Complete tear of the ligament with severe instability.
Dr. Mazzara recommends all grade 3 PCL injuries be treated surgically due to the low likelihood of healing. Successful surgical treatment happens ideally, within two to three weeks after the injury. This allows for early range of motion to make certain that sutures can be held into the torn structures with early motion after surgery.
How is a Posterolateral Corner Injury Treated?
Severe posterolateral corner injuries often require surgery to repair the soft tissue damage, including any tendons and ligaments involved in the injury. This surgery is typically done as an open procedure to repair or reconstruct the knee joint. Dr. Mazzara may use a graft for reconstruction which can be taken from the patient’s own body (autograft) or from a donor (allograft). The graft is secured to the outer surface of the femur (leg bone) and through the head of the fibula (smaller bone in the lower leg) with special surgical screws and sutures.
If you have questions about the treatment for a posterolateral corner injury or if you have knee instability, please contact the orthopedic offices of Dr. James Mazzara, knee specialist in Manchester, South Windsor, Enfield, Glastonbury and surrounding Hartford communities.