Reference, adapted, with permission, from one of the best shoulder sites on the web, www.shoulderdoc.co.uk.
What is a SLAP lesion?
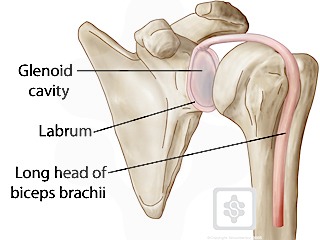
The shoulder is a ball-and-socket type of joint and is anatomically referred to as the glenohumeral joint, describing the two bony structures involved. The socket is the glenoid cavity, a cup-shaped piece of bone that juts out from a corner of the shoulder blade (scapula). The rim of the glenoid is formed by cartilage called the labrum. The ball that fits into the socket is the head (upper part) of the humerus (arm bone).
The upper (superior) part of the labrum anchors one of the two tendons of the biceps muscle. The feature that makes SLAP possible is the way the upper biceps tendon hooks over the head of the humerus. If the arm is forcefully bent inward and twists at the shoulder, the humeral head acts as a lever and tears the biceps tendon and labrum glenoid bone in a front-to-back (anterior-posterior) direction. And that is how the name SLAP is derived – Superior Labrum Anterior-Posterior or, in plain English, Upper Rim Front-Back. cartilage from the
SLAP area and SLAP Lesion – pull-off of the Biceps origin (superior labrum) from the glenoid.
Causes and Risk Factors
Often an initial forceful movement of the labrum attached to the biceps tendon to be torn away from the bone (glenoid). This may be associated with a dislocation of the joint, but commonly occurs in athletes and workers with a pull on the arm, weightlifting, throwing injury or tackle. Laborers can tear the labrum with a slip and fall while holding on a railing with the injured arm. If the initial condition does not heal properly, pain will result and worsen over time.
The typical symptoms are pain at the top of the shoulder, clicking and pain with overhead activities. These may be confused with AC Joint problems , but athletes with SLAP tears have pain with eccentric biceps loading (such as going down in a bench press). AC Joint pain is usually felt when pressing out at the end of a shoulder or bench press.
Risk Factors: Overhead and contact sports pose a greater risk of labral tears (SLAP lesions). Workers performing heavy lifting or pulling tasks are also at risk. Sudden traction injuries to the arm are common causes of SLAP lesions.
Types of SLAP Tears – Depending on the type and severity of injury, the labrum will tear in different ways and degrees. These are classified as a guide to treatment.
If you have been diagnosed with a SLAP tear, your surgeon may have called it a ‘Type 1 or 2 or 3, etc’. SLAP tears have been classified according to their severity of tear. Please note that it does not mean that the outcome of surgery is worse, it just gives us surgeons a guide to management and a form of communication. The common types are types 1 to 4. There are other types, but these are rare.
SLAP Type 1
This is a partial tear and degeneration to the superior labrum, where the edges are rough and fray along the free margin, but the labrum is not completely detached.
Treatment is usually to ‘debride’ (clean) the edges.
SLAP Type 2
Type 2 is the commonest type of SLAP tear. The superior labrum is completely torn off the glenoid, due to an injury. This type leaves a gap between the articular cartilage and the labral attachment to the bone. Type 2 SLAP tears can be further subdivided into (a) anterior (b) posterior, and (c) combined anterior-posterior lesions.
Treatment is reattachment of the labrum (SLAP repair). This is done arthroscopically using suture anchors. Recent data suggests that type 2 SLAP lesions do very well with a debridement and biceps tenodesis rather than repair of the labrum. Tenodesis seems to be associated with a lower rate of complications and a faster return to work. Many shoulder surgeons limit SLAP repairs to overhead throwing athletes.
SLAP Type 3
A Type 3 tear is a ‘bucket-handle’ tear of the labrum, where the torn labrum hangs into the joint and causes symptoms of ‘locking’ and ‘popping’ or ‘clunking’.
Treatment usually involves removal of the ‘bucket-handle’ segment and then repair of any remaining detached, unstable labrum (SLAP repair). This is done arthroscopically using suture anchors.
Biceps tenodesis seems to be associated with a lower rate of complications and a faster return to work. Many shoulder surgeons limit SLAP repairs to overhead throwing athletes.
SLAP Type 4
The Type 4 SLAP tear is one where the tear of the labrum extends into the long head of biceps tendon. Treatment is reattachment of the labrum (SLAP repair) and repair of the biceps tear, or a biceps tenodesis. This is done arthroscopically using suture anchors.

Prevention of SLAP lesions
Strong shoulder muscles remain the best defense against shoulder injuries. Exercises that build up these muscles around the shoulder should be done. Adequate warm-up before activity and avoidance of high-contact sports will help prevent of an instability-causing injury.
Treatment
Painkillers and anti-inflammatories – help control the pain.
Physical therapy can be helpful is some cases of SLAP lesions and should be considered if shoulder motion is limited or if there is weakness of the shoulder related to the initial injury.
Surgery may be recommended if an patient wants to continue their work, sports and training – SLAP lesions are sometimes repaired by arthroscopically through 2 or 3 small incisions. Some SLAP lesions can be simply debrided and cleaned, while most need repairing depending on the severity of the lesion. The associated lesions are also treated such as labrum and ligament lesions with instability.
You can see an animation of a SLAP repair on my website here. Go to the shoulder section and select SLAP repair.
Try this link as well for a SLAP repair.
Recent data and reports suggests that the only patients who should have their SLAP lesion repaired should be overhead throwing athletes. Other with SLAP lesions seem to have superior outcomes with an arthroscopic debridement and tenodesis of biceps tendon.
Biceps Tenodesis
In this procedure the long head of the biceps tendon is detached from it’s attachment in the shoulder and reattached to the humerus bone just below the shoulder. This procedure is more complex than a tenotomy, but avoids the risks of biceps discomfort (rare), and a ‘popeye’ appearance of the biceps muscle. Weakness is usually not a problem after biceps tenotomy.
Tenodesis, rather than tenotomy, may be preferable for more active, younger, thinner patients and those concerned about the appearance of the arm after surgery. Using modern fixation screws the repair is strong enough to move the arm early after surgery, without immobilization.
The Procedure:
1. The long head of the biceps tendon is released via the arthroscope:


arthroscopic scissors inserted via small puncture hole in skin and cutting the long head of biceps (arthroscopic view on the right).
2. A small incision (5cm) is made over the front of the shoulder and the tendon retrieved through this hole:


3. The tendon is fixed back into the bone of the humerus with a special interference screw:



Information before your surgery
You must not eat or drink anything after midnight the day before your surgery. When you wake up following the procedure you will be wearing a sling with a body belt. The sling should be worn for a few days to up to 6 weeks depending on the procedure performed and the time required for healing.
You will probably not be in hospital overnight after your operation, and should be able to go home about 4 hours after the surgery. Your may be given some exercises on your post operative discharge instructions and instructions on when to begin them.
At your first post operative visit in the office, I will review the procedure performed and your restrictions. You should also prepare to see the physical therapist in the office who will teach you the appropriate exercises. You will need physiotherapy after the surgery and should return to your own therapist.
Pain
A nerve block is usually used during the surgery. This means that immediately after the operation the shoulder and arm often feel completely numb. This may last for a few hours. After this the shoulder may well be sore and you will be given painkillers. These can be continued after you are discharged home. Ice packs or a cold compression wrap may also help reduce pain. Wrap crushed ice or frozen peas in a damp, cold cloth and place on the shoulder for up to 15 minutes. Ensuring you cover the wound site with a piece of gauze and tape to keep the area dry.
Wounds
This arthroscopic operation is usually done through two or three 5mm puncture wounds. There may be stitches under the skin and there may be paper strips over the wounds. These can be kept dry until healed. In some cases, I will give you permission to shower and get the wounds wet after surgery. It depends on the size of the incision.
Sleeping
For the first 3 – 6 weeks your sling must be worn in bed. Sleeping can be uncomfortable if you try and lie on the operated arm. We recommend that you lie on your back or on the opposite side, as you prefer.
Sleeping in a reclined position in a reclining chair or on a couch surrounded by pillows is usually the most comfortable position.
Ordinary pillows can be used to give you comfort and support. If you are lying on your side one pillow slightly folded under your neck gives enough support for most people. A pillow folded in half supports the arm in front and a pillow tucked along your back helps to prevent you rolling onto the operated shoulder during the night. If you are lying on your back, tie a pillow tightly in the middle (a “butterfly pillow”) or use a folded pillow to support your neck. Place a folded pillow under the elbow of the operated arm to support that.
Follow up appointments
An appointment will be made for you to see the me in the office on the first office day after surgery.
Daily activities
After a SLAP repair, for the first three weeks all activities of daily living for example feeding, dressing, cooking etc must be carried out using your un-operated arm. If appropriate an physical therapist will be available to give you advice on how to do this. Activities may also be limited for as long as 6 weeks after a repair. My patients usually see the therapist at the first post op visit the day after surgery.
If you had a SLAP debridement and biceps tenodesis (reattachment of the biceps to the upper humerus), I usually allow patients to move the shoulder immediately after surgery. You may not use the operative arm / hand to lift or pull anything since this may result in a rupture of the biceps tenodesis. Moving the shoulder is permitted.
If you had a SLAP debridement and biceps tenotomy (biceps cut and released and not repaired), you may use the arm as tolerated without restrictions immediately after surgery. You activities are limited by you pain.
Your physical therapist and surgeon will advise you when it is safe to resume your leisure activities. This will vary according to your sport and level, as well as the period required to retrain your shoulder muscles with physical therapy.
Driving
You may not be able to drive for a minimum of 4 weeks. Your surgeon will confirm when you may begin.
Return to work
This will depend upon whether the SLAP lesion was repaired, which requires additional healing time or whether a SLAP debridement and biceps tenodesis was performed.
In my experience, patients may return to work sooner if they have had a debridement and tenodesis or tenotomy than those who have had a SLAP repair. Patients having a SLAP repair seem to develop more stiffness and more post op discomfort than those having tenodesis of tenotomy.
You will need to discuss this with your surgeon.
Reference, adapted from one of the best shoulder sites on the web, www.shoulderdoc.co.uk.
Thanks for the reminder and permission, Prof. Funk.
Thanks,
JTM, MD